Compared to a routine dental filling or crown (cap), replacement of a missing tooth or teeth with implants is a more complicated and lengthy process. It will take several phases. A periodontist or an oral surgeon will place the implant surgically. Then we will place the tooth or visible portion.
Phase One
The specialist evaluates the position, suitability, and strength of the bone that will surround the implant. This information determines the length and width of the implants and how many implants will be necessary to replace the missing teeth. Impressions of all your teeth will be taken for study models in order to design the shape of the tooth or teeth to be implanted. A surgical guide will be made to indicate to the surgeon where the implants should be placed.
Phase Two
Surgical procedure is done to place the implant in the bone. A local anesthetic is given, and the gum tissue is lifted to expose the implant site. The implant is placed into the bone and the gum is closed over it. You will not see the implant while integration with the bone takes place. The integration takes 4 to 6 months. After this time, the site is opened again and a healing collar will be threaded into the implant. This will guide the tissue into a shape that is needed for the future crown(s). The time that the healing collar needs to be in place will vary from person to person, but will be at least several weeks.
Phase Three
Once the tissue shape is sufficient, specific attachments and components will be fitted to the implant. The implant components are similar in function to the wall or plaster anchors used to hang pictures on drywall. The healing collar is removed. Implants transfer copings, analogs, and other items are used to take an impression of the site. The healing collar is then put back on. The impressions and implant components are sent to the laboratory for fabrication of implant posts and temporary acrylic crowns.
When the temporary crown or bridge is returned from the laboratory, the healing collar is removed and the implant attachments are fasted to the implant. The temporary crowns are then seated and adjusted. They will be held in place by temporary cement or with screws, depending on your certain situation. We will explain the advantages and disadvantages of each in your particular case at the time you decide to have the implant
Temporary crowns are placed because the bone that supports and surrounds the implant must be given the opportunity to be put into function gradually. Implant techniques dictate that the implants be slowly brought into biting function. This means you will be returning several times to have more acrylic added to the temporary crown. After the implant and temporary crown have been in biting function for a few months, the final crown(s) will be fabricated and cemented or screwed into place.
Maintaining All Your Teeth
To keep your implants and your natural teeth healthy and functional for the longest time possible, clean the implant and your other teeth daily, as instructed. You will also need to come in for dental hygiene recare appointments at a 3- to 4-month interval. You have invested time and money in these state-of-the-art tooth replacements. Maintaining them as instructed will give you the best chance of success.
We feel that the benefits of replacing teeth with implant-supported crowns and bridges far outweigh the inconvenience of the long start to finish time. This is especially true when the teeth on either side of the implant are sound, unfilled teeth that would not otherwise require dental treatment. Implants help you preserve your nature tooth structure.
If you have any questions about dental implants, please feel free to ask us.
Friday, July 18, 2014
Implants: Procedural Overview
Labels:
austin,
cap,
crown,
dental,
dental implant,
dentist,
gum,
implant procedure,
implants,
missing teeth,
missing tooth,
omni dental,
periodontist,
screws,
teeth,
tooth
Thursday, July 17, 2014
A Beginner's Basics to Braces
How can orthodontics help you?
If your teeth are in poor alignment, you could be facing a functional or cosmetic problem. Orthodontics (braces) can eliminate that problem for you. One of the first things people notice about you is your smile and how your teeth look. You don't have to be a dentist to notice poorly positioned, crooked teeth. In today's culture, crooked teeth are not regarded as attractive or desirable. Most people, when asked, say that they would like to have straight teeth. Straight, white teeth are the cosmetic dental improvements patients most request.
Braces may also be suggested to correct a specific dental problem that only affects one or several teeth. This is not a cosmetic tooth repositioning, but rather a functional tooth movement. Occasionally, in order to properly finish an orthodontic case, the orthodontist may ask the dentist to adjust the enamel of some teeth or bond a resin to some teeth to improve the occlusion (bite alignment) or to enhance cosmetics. This will be discussed with you as soon as it becomes apparent.
When should you see an orthodontist?
 The need for orthodontics is best discovered when you are young. A dentist will have a good indication of whether or not your teeth will be straight when he sees you as a child 6 to 8 years of age. Most treatment would not begin until a patient is 8 years old, although in some cases, orthodontics can be started earlier.
The need for orthodontics is best discovered when you are young. A dentist will have a good indication of whether or not your teeth will be straight when he sees you as a child 6 to 8 years of age. Most treatment would not begin until a patient is 8 years old, although in some cases, orthodontics can be started earlier.
It is easier to direct the movement of teeth in a child. Early tooth guidance is a very important phase of orthodontic care, which can take place even though all the permanent teeth are not yet in place. Certain problems are much easier to correct at this stage of a "mixed dentition" of baby and permanent teeth. An average case can last from 18 to 24 months.

While orthodontic therapy is admittedly easier in the child patient, you are never too old to begin orthodontics. The number of adults seeking orthodontic treatment has risen dramatically during the past decade. As long as you have healthy bone support for your teeth, you can have orthodontic therapy. Most adult cases take 18 to 24 months to complete.
 What are retainers?
What are retainers?
Once braces are removed, it is usually necessary to wear a retainer. After your braces come off, your orthodontist will make a mold of your mouth and produce a set of retainers. This retainer will maintain the new tooth alignment until the teeth have had a chance to become firmly set in their new positions. This retainer may be either removable or fixed in place. Aside from a permanent bonded retainer, there are two other types that most people get.
A Hawley Retainer is made of acrylic and metal. The acrylic goes behind your teeth and up against your upper palate; the metal is in front of your teeth. This is the most reliable refinements that still need to be done to your teeth.
An Essix Retainer is clear plastic and looks like an Invisalign aligner tray. Many people want this type of retainer, but it has its disadvantages. Many orthodontists feel that because it covers the biting surface of your teeth, they do not "settle" properly after treatment. For this reason, sometimes orthodontists give a patient both types of retainers: an Essix Retainer to wear during the day when they are people-facing, and a Hawley Retainer to wear at night when they are home sleeping.
No matter what type of retainer you get, the most important thing is to wear it exactly as the orthodontist tells you. Most people need to wear their retainers 24/7 for at least 6 months, then switch to wearing it only at night when sleeping.
How do I keep clean teeth with braces on?
 While orthodontic treatment is in the active phase, that is, while the braces are on your teeth, you must be very diligent about keeping your teeth clean. This will be more difficult than and somewhat different from cleaning your teeth without braces. You will be instructed in the use of any cleaning aids needed. These may include dental floss threaders, orthodontic toothbrushes, an oral irrigator to flush out debris, proper brushing habits, fluoride mouth-rinses, and periodontal aids. You must follow your proper oral self-care routine each night to prevent decay, decalcification of the teeth, and gum disease. You also should not use a whitening toothpaste when you have braces. It could cause you to have "two tone" teeth after the brackets are removed. Another thing to remember is that although a device like a Waterpik is great for gum stimulation and dislodging food, it is not a substitute for flossing. You still need to floss daily.
While orthodontic treatment is in the active phase, that is, while the braces are on your teeth, you must be very diligent about keeping your teeth clean. This will be more difficult than and somewhat different from cleaning your teeth without braces. You will be instructed in the use of any cleaning aids needed. These may include dental floss threaders, orthodontic toothbrushes, an oral irrigator to flush out debris, proper brushing habits, fluoride mouth-rinses, and periodontal aids. You must follow your proper oral self-care routine each night to prevent decay, decalcification of the teeth, and gum disease. You also should not use a whitening toothpaste when you have braces. It could cause you to have "two tone" teeth after the brackets are removed. Another thing to remember is that although a device like a Waterpik is great for gum stimulation and dislodging food, it is not a substitute for flossing. You still need to floss daily.
If your teeth are in poor alignment, you could be facing a functional or cosmetic problem. Orthodontics (braces) can eliminate that problem for you. One of the first things people notice about you is your smile and how your teeth look. You don't have to be a dentist to notice poorly positioned, crooked teeth. In today's culture, crooked teeth are not regarded as attractive or desirable. Most people, when asked, say that they would like to have straight teeth. Straight, white teeth are the cosmetic dental improvements patients most request.
Braces may also be suggested to correct a specific dental problem that only affects one or several teeth. This is not a cosmetic tooth repositioning, but rather a functional tooth movement. Occasionally, in order to properly finish an orthodontic case, the orthodontist may ask the dentist to adjust the enamel of some teeth or bond a resin to some teeth to improve the occlusion (bite alignment) or to enhance cosmetics. This will be discussed with you as soon as it becomes apparent.
When should you see an orthodontist?
 The need for orthodontics is best discovered when you are young. A dentist will have a good indication of whether or not your teeth will be straight when he sees you as a child 6 to 8 years of age. Most treatment would not begin until a patient is 8 years old, although in some cases, orthodontics can be started earlier.
The need for orthodontics is best discovered when you are young. A dentist will have a good indication of whether or not your teeth will be straight when he sees you as a child 6 to 8 years of age. Most treatment would not begin until a patient is 8 years old, although in some cases, orthodontics can be started earlier.It is easier to direct the movement of teeth in a child. Early tooth guidance is a very important phase of orthodontic care, which can take place even though all the permanent teeth are not yet in place. Certain problems are much easier to correct at this stage of a "mixed dentition" of baby and permanent teeth. An average case can last from 18 to 24 months.

While orthodontic therapy is admittedly easier in the child patient, you are never too old to begin orthodontics. The number of adults seeking orthodontic treatment has risen dramatically during the past decade. As long as you have healthy bone support for your teeth, you can have orthodontic therapy. Most adult cases take 18 to 24 months to complete.
 What are retainers?
What are retainers? Once braces are removed, it is usually necessary to wear a retainer. After your braces come off, your orthodontist will make a mold of your mouth and produce a set of retainers. This retainer will maintain the new tooth alignment until the teeth have had a chance to become firmly set in their new positions. This retainer may be either removable or fixed in place. Aside from a permanent bonded retainer, there are two other types that most people get.
A Hawley Retainer is made of acrylic and metal. The acrylic goes behind your teeth and up against your upper palate; the metal is in front of your teeth. This is the most reliable refinements that still need to be done to your teeth.
 |
| Orthodontic Toothbrush |
No matter what type of retainer you get, the most important thing is to wear it exactly as the orthodontist tells you. Most people need to wear their retainers 24/7 for at least 6 months, then switch to wearing it only at night when sleeping.
How do I keep clean teeth with braces on?
 While orthodontic treatment is in the active phase, that is, while the braces are on your teeth, you must be very diligent about keeping your teeth clean. This will be more difficult than and somewhat different from cleaning your teeth without braces. You will be instructed in the use of any cleaning aids needed. These may include dental floss threaders, orthodontic toothbrushes, an oral irrigator to flush out debris, proper brushing habits, fluoride mouth-rinses, and periodontal aids. You must follow your proper oral self-care routine each night to prevent decay, decalcification of the teeth, and gum disease. You also should not use a whitening toothpaste when you have braces. It could cause you to have "two tone" teeth after the brackets are removed. Another thing to remember is that although a device like a Waterpik is great for gum stimulation and dislodging food, it is not a substitute for flossing. You still need to floss daily.
While orthodontic treatment is in the active phase, that is, while the braces are on your teeth, you must be very diligent about keeping your teeth clean. This will be more difficult than and somewhat different from cleaning your teeth without braces. You will be instructed in the use of any cleaning aids needed. These may include dental floss threaders, orthodontic toothbrushes, an oral irrigator to flush out debris, proper brushing habits, fluoride mouth-rinses, and periodontal aids. You must follow your proper oral self-care routine each night to prevent decay, decalcification of the teeth, and gum disease. You also should not use a whitening toothpaste when you have braces. It could cause you to have "two tone" teeth after the brackets are removed. Another thing to remember is that although a device like a Waterpik is great for gum stimulation and dislodging food, it is not a substitute for flossing. You still need to floss daily.
Labels:
austin,
braces,
brackets,
cosmetic,
crooked teeth,
dental,
dentist,
essix,
floss,
flossing,
hawley,
metal,
omni dental,
orthodontist,
retainer,
straight teeth,
toothbrush,
waterpik
Wednesday, July 16, 2014
How Do Dentists Fix A Chipped Tooth
 If you have chipped your tooth, do not worry - you can get your chipped tooth fixed to look brand new by cosmetic dental procedures. A dentist who is trained in cosmetic and restorative procedures will make it look life-like and aesthetic, that you yourself couldn't tell a difference.
If you have chipped your tooth, do not worry - you can get your chipped tooth fixed to look brand new by cosmetic dental procedures. A dentist who is trained in cosmetic and restorative procedures will make it look life-like and aesthetic, that you yourself couldn't tell a difference.A chipped tooth generally means that a small flake of your tooth surface is chipped off. Usually, it is the front tooth (these are used more to open bottles and bite on hard things). You can get a chipped tooth corrected easily and pain-free by a sitting in a single procedure called composite bonding. There are a few other procedures to correct a chipped tooth, but composite bonding is the most efficient, easy, aesthetic, and cost effective.
What is composite bonding?
Composite bonding is dental restorative procedure to restore the aesthetic and function of a tooth which may have broken due to any trauma or decay.
What is composite?
Composite is a mixture of different materials that are combined together to enhance and complement each other's properties. Composite is primarily made up of synthetic resins, filler particles, shade producing agents, chemical initiators and inhibitors, and much more.
1. Adhesive
2. Etchant
3. Composite Syringes
Composite is packed in a syringe-like tube and comes out in a semi-solid form. This semi-solid paste-like substance is used to build up the chipped portion of the tooth.
Method of Composite Bonding to Fixed a Chipped Tooth
1. Tooth is cleaned with prophylaxis paste
2. Chipped area and sharp margin is slightly smoothened
3. Chipped area is treated with an etchant (blue-colored gel)
4. Tooth surface is blotted and a layer of adhesive is applied (bonds the composite with tooth). A blue-colored light will be shown over the tooth surface from a curing light equipment (it cures the adhesive layer)
5. Composite is applied layer by layer and cured by the blue-colored light
6. Proper tooth anatomy is restored in the chipped area by incremental buildup of the composite
7. Composite is polished
8. A mirror will be given to you to see the work
Time and Cost
The procedure takes about 45 minutes, depending on difficulty level. The cost may be anywhere between $150 to $500. The cost may go on the higher side depending upon the status and skill of the dentist.
If your tooth has a large amount of tooth structure loss, then your dentist may suggest veneers or crowns for proper strength and buildup.
http://www.drpulp.com/2013/07/how-to-fix-chipped-tooth.html
Fixed and Removable Orthodontics
The traditional and stereotypical movie, television, and commercial vision of orthodontic treatment is one of yards of metal wire tied down to teeth so covered with silver bands and brackets that the whites of the teeth are barely visible. With today's advanced dental technology, this picture is far from accurate.
Tooth Alignment:
Changes in tooth alignment can be accomplished in several different ways. When appropriate, upper and lower arch expanders can be used to increase the curvature of the tooth-bearing supporting structures. These expanders are usually cemented into place and are not able to be removed by the patient. The expanders are often a prelude to fixed metal bands. They can be cemented to the teeth as well as longitudinal arch wires and springs and still be used to move teeth.
 The look:
The look:
Some time ago, the desire of patients to show less metal resulted in the development of bonded tooth-colored and clear brackets (as opposed to the metal bands that completely surround a tooth). These brackets cover only about 25% of the tooth surface and are bonded into place. The trade-off with the more esthetic bonded brackets is a higher percentage of dislodgement of the bracket, requiring additional office visits for repair and replacement. The wires and springs are changed periodically to accomplish the various stages of movement. The metal components stay in place until the tooth movement is finished. Some dental conditions mandate the use of this traditional orthodontic process.
Removable:
It is not always necessary to use fixed devices to move teeth. Less aggressive tooth movement can additionally be done with patient-removable appliances. Some are made of a gum-colored pink acrylic material with metal wires and springs embedded in them. These are worn by the patient except when he or she is eating, brushing, and flossing. The metal and plastic appliances do not show as much metal so they are somewhat more acceptable. The trade-off with removable appliances is that they only work when they are in the patient's mouth, making proper patient compliance a big issue. If you do not wear them, the teeth will not move as planned. The metal and plastic appliances are used in what is called minor tooth movement. Many orthodontic cases are not appropriate for removable appliance therapy.
Invisalign:
Several years ago, a new type of removable appliance therapy was developed and patented. Align Technology has a product called Invisalign. Clear, thin plastic aligners (positioners) are sequentially placed to move the teeth in a precise fashion. The aligners are left in the mouth as much as possible and removed only for eating, drinking, and cleaning the teeth. Again, if you do not wear them, the teeth will not move. The aligners are almost invisible when in place and are extraordinarily acceptable esthetically. They are indicated for adults and patients older than 14 years who have all permanent teeth in including fully erupted second molars. They can be used to treat simple to fairly extensive misalignment problems. Most cases are completed in about 12 months. Research is still in progress to determine the limits of this process.
The doctor who will be performing the orthodontic treatment will take these different modalities into consideration and develop a treatment plan best suited to your needs. Age of the patient, number of teeth involved, and extent of movement are primary factors in the decision-making process. Please be sure to ask why or why not one technique rather than another was suggested.
If you have any questions about your orthodontic treatment, please feel free to ask us.
Tooth Alignment:
Changes in tooth alignment can be accomplished in several different ways. When appropriate, upper and lower arch expanders can be used to increase the curvature of the tooth-bearing supporting structures. These expanders are usually cemented into place and are not able to be removed by the patient. The expanders are often a prelude to fixed metal bands. They can be cemented to the teeth as well as longitudinal arch wires and springs and still be used to move teeth.
 The look:
The look: Some time ago, the desire of patients to show less metal resulted in the development of bonded tooth-colored and clear brackets (as opposed to the metal bands that completely surround a tooth). These brackets cover only about 25% of the tooth surface and are bonded into place. The trade-off with the more esthetic bonded brackets is a higher percentage of dislodgement of the bracket, requiring additional office visits for repair and replacement. The wires and springs are changed periodically to accomplish the various stages of movement. The metal components stay in place until the tooth movement is finished. Some dental conditions mandate the use of this traditional orthodontic process.
Removable:
 |
| Tooth-colored Braces |
Invisalign:
Several years ago, a new type of removable appliance therapy was developed and patented. Align Technology has a product called Invisalign. Clear, thin plastic aligners (positioners) are sequentially placed to move the teeth in a precise fashion. The aligners are left in the mouth as much as possible and removed only for eating, drinking, and cleaning the teeth. Again, if you do not wear them, the teeth will not move. The aligners are almost invisible when in place and are extraordinarily acceptable esthetically. They are indicated for adults and patients older than 14 years who have all permanent teeth in including fully erupted second molars. They can be used to treat simple to fairly extensive misalignment problems. Most cases are completed in about 12 months. Research is still in progress to determine the limits of this process.
The doctor who will be performing the orthodontic treatment will take these different modalities into consideration and develop a treatment plan best suited to your needs. Age of the patient, number of teeth involved, and extent of movement are primary factors in the decision-making process. Please be sure to ask why or why not one technique rather than another was suggested.
If you have any questions about your orthodontic treatment, please feel free to ask us.
Labels:
alignment,
austin,
braces,
brackets,
clear,
clear braces,
dentist,
expanders,
invisalign,
metal,
omni dental,
orthodontics,
removable,
removable braces,
straight teeth,
teeth,
tooth,
tooth alignment
Tuesday, July 15, 2014
Prevention of Decay
What is dental decay, and how do dentists fix it?
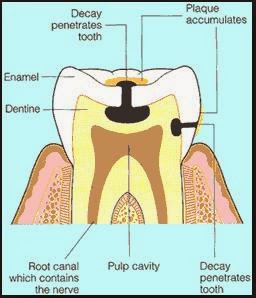
Dental caries (decay) is a bacterial infection, first of the enamel, then of the dentin of the tooth. The tradition in dentistry has been to surgically remove the diseased portion of the tooth by "drilling" out the decay and then filling the resulting hole in the tooth with some inert material. As most adults know, this procedure will be performed over and over again when new decay begins or when the filling (often silver) breaks or the tooth fractures.
Click here to learn about decay in young children.
Why should I practice prevention?
Would it not be better to eliminate the cause of the infection and thus not be forced to have big holes drilled in the teeth? We believe the bacterial cause of the infection should be addressed.
How do I prevent dental decay?
There are several positive steps that you can take to reduce your risk of dental decay.
A. At the dentist's office
1. First, all the active decay in your mouth should be treated immediately.
2. Next, all teeth that would benefit from sealants should be treated.
4. We believe that the use of a fluoridated mouthrinse twice daily or use of a prescription fluoridated dentifrice as directed provides a great advantage.
B. In your daily life
6. Your diet and oral self-care are important in dental decay prevention. When you eat junk food and drink sugary liquids, your teeth are more prone to decay. The more frequently you snack, the more prone your teeth will be to decay.
 7. If your brushing and flossing are not effective, your teeth will be more prone to decay. When you can't brush after a meal, at least rinse your mouth with water within 15 minutes to dilute the acids forming from the ingested food or drink.
7. If your brushing and flossing are not effective, your teeth will be more prone to decay. When you can't brush after a meal, at least rinse your mouth with water within 15 minutes to dilute the acids forming from the ingested food or drink.
8. If you have a diminished salivary flow, take frequent sips of water during the day to help dilute the acids produced by the bacteria.
What if decay keeps coming back?
If you have a continuing problem with active decay, we recommend more frequent preventive recare appointments. It has been repeatedly shown that patients who have good oral self-care and maintain a recare interval of 3 to 4 months have many fewer dentally related (cavities or gum disease) problems.
Present-day dental suggestions are based on proven scientific information. You might need to have your teeth cleaned by the hygienist twice each year, or you may need to be seen more frequently.
For certain individuals, we also suggest testing the oral bacterial levels to determine the magnitude and presence of a Streptococcus mutans infection and to determine your risk level for future dental disease.
If you have any questions about the prevention of dental decay, please feel free to ask us.
Dental caries (decay) is a bacterial infection, first of the enamel, then of the dentin of the tooth. The tradition in dentistry has been to surgically remove the diseased portion of the tooth by "drilling" out the decay and then filling the resulting hole in the tooth with some inert material. As most adults know, this procedure will be performed over and over again when new decay begins or when the filling (often silver) breaks or the tooth fractures.
Click here to learn about decay in young children.
Why should I practice prevention?
Would it not be better to eliminate the cause of the infection and thus not be forced to have big holes drilled in the teeth? We believe the bacterial cause of the infection should be addressed.
How do I prevent dental decay?
There are several positive steps that you can take to reduce your risk of dental decay.
A. At the dentist's office
1. First, all the active decay in your mouth should be treated immediately.
2. Next, all teeth that would benefit from sealants should be treated.
- Why? This will prevent bacteria from reaching into the pits, fissures, and grooves that normally exist on the occlusal (biting) surfaces of teeth. Any stray bacteria that may still be in the sealed area are effectively cut off from their source of food and become inactive. Although sealants are most effective on teeth that have not been previously restored, they can be successfully placed on teeth filled with bonded fillings.
4. We believe that the use of a fluoridated mouthrinse twice daily or use of a prescription fluoridated dentifrice as directed provides a great advantage.
- Why? Not only is fluoride effective against bacteria but it also creates an environment that promotes remineralization of slightly damaged enamel. The decay process is reversed, and the tooth may not have to be drilled.
B. In your daily life
6. Your diet and oral self-care are important in dental decay prevention. When you eat junk food and drink sugary liquids, your teeth are more prone to decay. The more frequently you snack, the more prone your teeth will be to decay.
 7. If your brushing and flossing are not effective, your teeth will be more prone to decay. When you can't brush after a meal, at least rinse your mouth with water within 15 minutes to dilute the acids forming from the ingested food or drink.
7. If your brushing and flossing are not effective, your teeth will be more prone to decay. When you can't brush after a meal, at least rinse your mouth with water within 15 minutes to dilute the acids forming from the ingested food or drink. 8. If you have a diminished salivary flow, take frequent sips of water during the day to help dilute the acids produced by the bacteria.
What if decay keeps coming back?
If you have a continuing problem with active decay, we recommend more frequent preventive recare appointments. It has been repeatedly shown that patients who have good oral self-care and maintain a recare interval of 3 to 4 months have many fewer dentally related (cavities or gum disease) problems.
Present-day dental suggestions are based on proven scientific information. You might need to have your teeth cleaned by the hygienist twice each year, or you may need to be seen more frequently.
For certain individuals, we also suggest testing the oral bacterial levels to determine the magnitude and presence of a Streptococcus mutans infection and to determine your risk level for future dental disease.
If you have any questions about the prevention of dental decay, please feel free to ask us.
Labels:
austin,
brushing,
caries,
cavity,
decay,
dentin,
dentist,
eating,
enamel,
filling,
flossing,
fluoride,
omni dental,
prevention,
sealants,
teeth,
tooth,
tooth decay
Monday, July 14, 2014
Extractions
Reasons for Recommending Tooth Extraction
Teeth may need to be extracted for several reasons, including but not limited to:
The Procedure
1. Numb the tooth: Your dentist will need to anesthetize (numb up) both your tooth and the bone and gum tissue that surround it. This is done as an injection.
 2. Extraction: The root portion of a tooth is firmly encased in bone (its socket), and tightly held in place by a ligament. During the extraction process, the dentist needs to both "expand the socket" (widen and enlarge it) and separate the tooth from its ligament, to the point where the tooth is loose and free to come out.
2. Extraction: The root portion of a tooth is firmly encased in bone (its socket), and tightly held in place by a ligament. During the extraction process, the dentist needs to both "expand the socket" (widen and enlarge it) and separate the tooth from its ligament, to the point where the tooth is loose and free to come out.
1. Dental Elevators: During the extraction process, a dentist will usually use an elevator first. These instruments are designed to be wedged in the ligament space between the tooth and its surrounding bone. As the elevator is forced and twisted, the tooth is pressed and rocked against the bone. This helps to expand the socket. It also helps to separate the tooth from its ligament. As this work is continued, the tooth will become more and more mobile. In some cases, the elevator may be able to shove the tooth on out. If not, the dentist will switch to the use of extraction forceps and remove the tooth with them.
2. Extraction Forceps: A dentist will usually keep a number of different extraction forceps on hand. Each one will have a design that's been specially made to grasp a certain type of tooth. When they're used, the dentist will grasp the tooth with the forceps and them firmly and deliberately rock it back and forth as much as it will. Because the bone that surrounds the tooth is compressible, the socket will expand. In addition to a rocking motion, a dentist will also rotate the tooth back and forth. This twisting action helps to rip and tear the tooth from the ligament that binds it in place. At some point, the socket will be enlarged enough, and the ligament torn enough, that the tooth can be easily removed.
What will I feel?
1. Pressure
2. You should not feel any pain
3. Expect to hear startling extraction noises: These are often just routine
Following the Extraction
We will tell you the reason for the extraction and let you know what to expect following the procedure. Please follow the instructions given to you. If antibiotics are prescribed, take them until the prescription is completely finished. If pain medication is prescribed, take it only if necessary. If the medication prescribed contains a narcotic component, such as codeine, do not drive a motor vehicle or operate machinery that could prove dangerous to yourself or others. Expect some bleeding to occur from the extraction site for the first 24 hours. Remember, there is now a hole in your jaw from which the tooth has been removed, and the hole can be quite large. Some bleeding is to be expected.
Teeth may need to be extracted for several reasons, including but not limited to:
- severe periodontal disease
- irreversible damage to the nerve tissue inside the tooth (and the patient decides against saving the tooth)
- failed endodontic therapy
- extreme fracture or decay of the tooth structure
- improper positioning of the tooth or for orthodontic purposes
The Procedure
1. Numb the tooth: Your dentist will need to anesthetize (numb up) both your tooth and the bone and gum tissue that surround it. This is done as an injection.
 2. Extraction: The root portion of a tooth is firmly encased in bone (its socket), and tightly held in place by a ligament. During the extraction process, the dentist needs to both "expand the socket" (widen and enlarge it) and separate the tooth from its ligament, to the point where the tooth is loose and free to come out.
2. Extraction: The root portion of a tooth is firmly encased in bone (its socket), and tightly held in place by a ligament. During the extraction process, the dentist needs to both "expand the socket" (widen and enlarge it) and separate the tooth from its ligament, to the point where the tooth is loose and free to come out.- What does it mean to "expand" a tooth's socket? If you have ever tried to remove a tent stake that has been driven deeply into the ground, you know that you can't just pull the stake straight up. Instead, you first have to rock the stake back and forth, widening the hole in which it is lodged. Once the hole has been enlarged enough, the stake will come out easily.
- How does the dentist expand the jaw bone? The bone inside the jaw is spongy. When a dentist applies firm pressure to a tooth (forcing it against the side of its socket), the bone will compress. After repeated application of pressure, from many different angles, the entire socket gradually becomes expanded. At some point, enough space will have been created (and the ligament separated from the tooth enough) that the tooth will come out.
- Removing infected or pathologic tissue by curetting (scraping) the walls of the tooth socket
- Using finger pressure to re-compress the "expanded" socket
- Rounding off sharp bone edges
- Evaluating the tooth socket for sinus complications (upper back teeth)
- Washing out ("irrigating") the socket, so to remove any loose bone or tooth fragments that remain
- Placing stitches (usually only after surgical extractions).
- Placing folded gauze over your extraction site and then having you bite down on it so to create firm pressure
1. Dental Elevators: During the extraction process, a dentist will usually use an elevator first. These instruments are designed to be wedged in the ligament space between the tooth and its surrounding bone. As the elevator is forced and twisted, the tooth is pressed and rocked against the bone. This helps to expand the socket. It also helps to separate the tooth from its ligament. As this work is continued, the tooth will become more and more mobile. In some cases, the elevator may be able to shove the tooth on out. If not, the dentist will switch to the use of extraction forceps and remove the tooth with them.
2. Extraction Forceps: A dentist will usually keep a number of different extraction forceps on hand. Each one will have a design that's been specially made to grasp a certain type of tooth. When they're used, the dentist will grasp the tooth with the forceps and them firmly and deliberately rock it back and forth as much as it will. Because the bone that surrounds the tooth is compressible, the socket will expand. In addition to a rocking motion, a dentist will also rotate the tooth back and forth. This twisting action helps to rip and tear the tooth from the ligament that binds it in place. At some point, the socket will be enlarged enough, and the ligament torn enough, that the tooth can be easily removed.
What will I feel?
1. Pressure
2. You should not feel any pain
3. Expect to hear startling extraction noises: These are often just routine
Following the Extraction
We will tell you the reason for the extraction and let you know what to expect following the procedure. Please follow the instructions given to you. If antibiotics are prescribed, take them until the prescription is completely finished. If pain medication is prescribed, take it only if necessary. If the medication prescribed contains a narcotic component, such as codeine, do not drive a motor vehicle or operate machinery that could prove dangerous to yourself or others. Expect some bleeding to occur from the extraction site for the first 24 hours. Remember, there is now a hole in your jaw from which the tooth has been removed, and the hole can be quite large. Some bleeding is to be expected.
- Do not spit, rinse, or smoke for 24 hours
- Do not drink through a straw for 24 hours
- It would be a good idea not to brush near the extraction site for a day or two
- When you brush and floss the area, be gentle!
- For 24 hours after the extraction, try to chew food away from the extraction site
- Some slight swelling in the area is to be expected, especially if the extraction was difficult
- If sutures are placed, return to have them removed
- If medication has been prescribed for possible post extraction discomfort, take it as directed
- If prescription medication has NOT been given, you may take your usual over-the-counter pain reliever, as directed

- There is extended bleeding from the extraction site. Slight bleeding for several hours is normal.
- Anything other than slight swelling occurs.
- Discomfort continues for more than 24 hours, especially if it is not relieved by over-the-counter pain relievers.
- fracture of adjacent teeth or restorations (which of course would mean that these affected areas must be restored to normal function after the healing of the extraction site)
- separated root tips or root fragments
- temporary or permanent nerve damage to the area, resulting in anesthesia or paresthesia (numbness)
- incomplete healing, resulting in severe pain - a "dry socket"
- fracture of the surrounding bone
Labels:
anesthesia,
austin,
bleeding,
decay,
dental elevator,
endodontic therapy,
extraction,
extraction forceps,
numbing,
omni dental,
pain,
periodontal disease,
suture,
swelling,
teeth,
tooth,
tooth extraction
Friday, July 11, 2014
Gingival Grafts
 What is it?
What is it? Periodontal (gum) surgery is most often associated with the removal of soft tissue. But there are times when it is necessary to use soft tissue to cover an area that has too little soft tissue remaining.
What causes it?
Exposed roots may be due to the improper brushing, periodontal disease, or genetic structure. Brushing too hard and/or with a hard toothbrush can cause the gingival tissue to disappear. The gingival margin (gumline) changes, and one or more millimeters of root structure can be exposed. Active periodontal disease can cause loss of this soft tissue too.
Why you should care
This exposure can lead to teeth that are very sensitive to temperature changes, root decay, or are quite unsightly. The disfigured soft tissue line can lead to a plaque trap, causing more disease and further problems.
How dentists fix it
Two methods of resolving these problems are free gingival grafts and attached gingival grafts. Both of these are periodontal surgical procedures. In both cases, a local anesthetic will be used to numb the treatment site.
In the case of an attached graft, gingival tissue is taken from the donor site and moved to the area where root coverage is required. The graft tissue is sutured into place, and a dressing is placed over the treated area. The dressing remains in place for several weeks and is then removed. An attached graft is not completely removed from the donor site. The donor site is adjacent to the site that needs root coverage. There is an incision made in the gum tissue, and the tissue is moved sideways, up, or down and sutured into place. Again, a protected dressing is placed to protect the area while healing occurs. Any anticipated postoperative discomfort is resolved with medication. Most discomfort will come from a free graft donor site.
Who performs the procedure?
A periodontist (gum specialist) usually performs these procedures, as well as other types of grafts and root coverage treatments. After the periodontist examines the areas needing treatment, you will have a better idea of what treatment will consist of, what the appearance may be, anticipated healing times, postoperative discomfort, and cost.
How can you prevent it?
Most patients have heard that they should take better care of their teeth - brush and floss the teeth. Some patients brush too hard and in a back-and-forth motion; and some facial, bony structures and biting forces are such that root exposure happens, resulting in longer looking teeth. The grafting procedures mentioned here can restore the proper gingival marginal architecture, prevent root decay, reduce or eliminate thermal sensitivity, and make your smile look great again.
If you have any questions about gingival grafts, please feel free to ask us.
Labels:
austin,
brushing,
decay,
flossing,
gingival graft,
graft,
gum graft,
gum recession,
gum surgery,
gums,
omni dental,
periodontal disease,
periodontics,
sensitivity,
soft tissue,
surgery,
teeth,
tooth
Subscribe to:
Posts (Atom)