Xerostomia (dry mouth) is not a condition everyone should
expect. You may notice it as you age due to a change in hormones, medication,
and/or radiation therapy in the head and neck region.
Why Xerostomia Is a
Problem
Saliva is important to oral health for several reasons. The
flow of saliva helps clear debris from the oral cavity. It provides minerals necessary
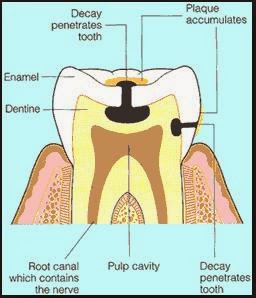
to support the process of remineralization. Tooth enamel daily undergoes acid
attack that removes inorganic minerals from teeth. This is called
demineralization. Remineralization is the opposite of demineralization. It
occurs when inorganic molecules flow into a region of weakened enamel and make
it stronger.
When the salivary flow is reduced, a chain of events occurs. The natural cleansing action is diminished, as are the buffering action and remineralization properties of saliva. People with diminished salivary flow experience a very fast rate of decay, many times faster and over several teeth. This type of dental decay is typically noted along the gumline, around existing dental work, and on exposed root surfaces.
Prevention
You can help prevent dental decay that can result from xerostomia:
- Brushing and flossing correctly twice a day becomes very important.
- Frequent sips of water during the day can help moisten the mouth and can help clear debris.
- Daily use of a mouthrinse containing fluoride can help remineralize teeth.
- Use a toothpaste containing sodium fluoride.
- We recommend a daily brushing with a prescription, high-concentration sodium fluoride gel or paste. We will either dispense this or give you a prescription for it.
- Chew sugarless gum or a rubber band to stimulate salivary flow.
- In moderate to severe cases, special fluoride delivery trays can be made for you to use at home. These will keep the high-concentration fluoride in a position to “soak” your teeth with fluoride for several minutes at a time.
- We recommend that you have your teeth cleaned, polished, and an office-applied topical fluoride treatment every 3 months while the condition persists.
Dry mouth can have serious dental consequences and must be
treated accordingly.
If you have any
questions about xerostomia, please feel free to contact us at any of our three
office locations:
Hymeadow: (512) 250-5012
Jollyville: (512) 346-8424
West William Cannon: (512) 445-5721